Electronic Discharge

Introduction
Patient safety has been listed as the first priority in the 2015 Health Service Executive (HSE) Service Plan and within the remit of patient safety, medication management is one the six key areas for focus (HSE, 2014). In 2007, the Irish government established The Commission on Patient Safety and Quality Assurance to develop clear and practical recommendations to ensure that safety and quality of care are paramount in the healthcare system (Madden, 2008). This change project is strongly influenced by the work of this commission, which recommended the establishment of the Health Information and Quality Authority (HIQA), the need for staff to participate in audit, implementation of evidence-based practice and more specifically the need to prioritise the introduction of medication reconciliation at transfers of care.
A six month pilot study commenced on the 11th January 2016 at Naas General Hospital and St. Luke’s Kilkenny to evaluate a new model of collaborative discharge medication reconciliation and computer generated discharge prescriptions. The purpose of this pilot is to improve medication safety at hospital discharge.
This case study outlines how the Electronic Discharge Prescription Pilot prevents medication errors using technology to handle medication reconciliation on admission and discharge to bring significant patient-centred benefits to the forenamed pilot sites.
The Challenge
Medication errors are consistently found to be of a high prevalence when adverse event data is analysed. The Harvard Medical Practice study conducted in fifty-one New York Hospitals found an adverse event rate of 3.7% from a review of 30,121 randomly selected patient records (NEJM, 1991). The most common type of incident was found to be drug complications at a rate of 19%, and the study also found that the incidence of adverse events rose with increasing age.
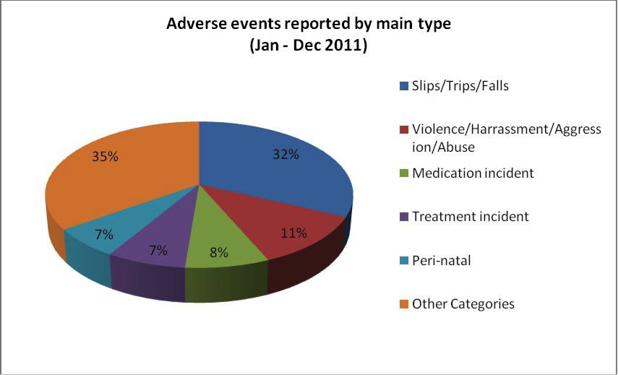
The Irish State Claims Agency has published a detailed breakdown of its data for 2011 (SCA, 2012). Medication incidents were the third highest category of adverse events at 8% of the total reported.
Within the medication incidents reported, it is notable that medication non-reconciliations at transfers of care were the second highest category following dosing errors. Given the aging population and the increasing incidence of patients who are on multiple medications, the risks associated with medication management at the interface are likely to worsen with time unless strategies to reduce risk are implemented (Moriarty, 2015; Lesar, 1997).
The Solution
Medication reconciliation has been defined as ‘the process of creating the most accurate list possible of all medications a patient is taking (including drug name, dosage and route) and comparing that list against the physician’s admission, transfer and/or discharge orders, with the goal of providing correct medication to the patient at all transition points within the hospital’ (www.ihi.org). A systematic review of hospital-based medication reconciliation practices found that from the 26 studies reviewed, there was a consistent reduction in medication discrepancies, potential adverse drugs events and adverse drug events (Mueller, 2012). A National Standard for Patient Discharge Summary Information was published in 2013 and includes the need for a complete and accurate list of medicines on discharge along with the information to support the changes to medication during the hospital admission (HIQA, 2013).
The eClinical Pharmacy Suite is a browser based application developed by Whathealth and exclusively licensed by Pfizer Healthcare Ireland.
The primary objective of the “eClinical Pharmacy Suite” is to support the role of the clinical pharmacist within hospital pharmacy with the provision of a suite of applications that can enable the:
• Registration of interventions in a structured, uniform manner
• Optimisation of medicine use
• Reduction of overuse, misuse and under use of medicines
To facilitate the requirements of this pilot, Pfizer collaborated with NGH to advance the software to handle:
• Drug Reconciliation at admission and discharge
• Produce a computer-generated prescription
The Software has completed a full security evaluation by the HSE’s Office of the Chief Information Officer and fully complies with all HSE Data Protection, Encryption and Password Polices.

The Journey so far…
The pilot kicked off in Naas General Hospital (NGH) and St. Luke’s Hospital, Kilkenny (SLK), on the 11th January 2016. Both centres are focusing on patient safety in high risk areas:
• Patient population (70+ and stroke) – NGH
• Prescribed 9 or more medications, at the time of admission. -NGH
• 2 x Medical wards and Acute Stroke Unit -SLK
• All patients of 3 x geriatricians admitted to these wards
Specific to NGH, a retrospective audit was completed for 30 discharge prescriptions, written August to November 2015, against the HIQA National Standard for Patient Discharge Summary Information 2013. The pilot in NGH is being conducted as part of the Masters in Leadership Program at the RCSI under the supervision of Dr Philippa Ryan-Withero, Deputy Chief Nursing Officer at the Department of Health.
A baseline audit was completed for 30 discharge prescriptions, written November and December 2015, against the HIQA National Standard for Patient Discharge Summary Information 2013
From the 11th January 2016 to the 5th February 2016:
30% of patients received a pharmacist-generated discharge prescription (computerised) and collaborative medication reconciliation between the pharmacist and the doctor at the time of discharge.
By the 1st March 2016:
An audit will be completed for all discharge prescriptions for patients receiving the new service against the HIQA National Standard for Patient Discharge Summary Information 2013.
An average time taken for pharmacist activity per discharge episode will be calculated.
This figure will be used to calculate an average cost per discharge using the HSE pharmacist salary scale.
The average number of medicines prescribed per discharge prescription will also be calculated
Specific to SLK:
Meds Rec on Admission and Discharge undertaken
Discharge process must be completed prior to patient leaving hospital
Copy of Discharge Prescription communicated to GP and Community Pharmacy
Healthlink email used in this process
Currently GP only
Potential for use by Community Pharmacy
Benefits for all
Patients:
Improved safety – less medication errors through the delivery of a medication reconciliation process and the provision of an electronic computer generated prescription
Improved patient knowledge and awareness of their prescribed medications
GPs
Improved communication and transparency on modifications made to patients prescription
Electronic Discharge Prescription avoids “illegible” issues that requires GPs time to follow up with hospital and seek clarification
Heathlink offers direct secured link to share updated Electronic Discharge Prescription to GPs
Hospitals
Effective and consistent Patient Discharge Management pathway
Electronic Discharge Prescription is a time saving process as it is much faster to produce compared to static paper based systems
Improved patient safety – the prescription is legible, contains standard and mandatory information on the identity of the patient and an update of the patients medication review that is updated in the hospitals records and shared with their GP
Conclusions
The pilot will conclude early July 2016 and early insights already demonstrate some of the key deliverables of the eHealth Ireland Knowledge and Information strategy:
Care Delivery Enablement – It provides a clinical and care delivery capability: the generation of electronic discharge prescriptions which was previously a manual process, thereby allowing electronic data capture, better quality of care, potentially more clinician time spent with the patient and a greater ability for patients to participate in their own care
Cross Setting Information Integration
Health Service Intelligence
The next steps
The 6 month pilot was endorsed by Mr. Richard Corbridge, CIO of the HSE, in December 2015. The purpose of the pilot study is to evaluate a new model of collaborative discharge medication reconciliation and computer generated discharge prescriptions as part of the discharge process in two controlled environments. On completion, the outcomes of the pilot study will be assessed to directly guide its suitability to scale up to a hospital group level.
Progress Update:
The team presented the attached poster at the European Association of Hospital Pharmacists (EAHP) which received very positive feedback. This poster provides a detailed update on the project and can be downloaded here. (GPI) Discharge Management: Safer Discharges and Improved Information Transfer Metrics
References
• Galvin, M., Jago-Byrne, M.C., Fitzsimmons, M. & Grimes, T. (2013) Clinical pharmacist’s contribution to medication reconciliation on admission to hospital in Ireland. International Journey of Clinical Pharmacy, 35: 14-21.DOI 10.1007/s 11096- 012-9696-1
• eClinical Pharmacy Suite
• Grimes, T. C., Duggan, C. A., Delaney, T. P., Graham, I. M., Conlon, K. C., Deasy, E., Jago-Byrne, M. C., O’Brien, P. (2011). Medication details documented on hospital discharge: Cross-sectional observational study of factors associated with medication non-reconciliation. Br J Clin Pharmacol. March 2011; 71 (3) 449-457. DOI: 10.1111/j.1365-2125.2010.03834x.
• HIQA (2013). National Standard for Patient Discharge Summary Information. www.HIQA
• Madden D. Building a culture of patient safety. (2008) Report of the commission of patient safety and quality assurance. Department of Health and Children
• Moriarty, Frank, et al. "Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross - sectional study." BMJ open 5.9 (2015): e008656.
• Mueller, Stephanie K., et al. "Hospital-based medication reconciliation practices: a systematic review." Archives of internal medicine 172.14 (2012): 1057-1069.
• Health Service Executive (2014). Health Service National Service Plan 2015. Dublin: Health Service Executive. www.hse.ie/serviceplan2015
• www.ihi.org
• www.stateclaims.ie
Acknowledgements:
• Ms. Marie Claire Jago-Byrne, Chief Pharmacist, Naas General Hospital
• Mr. Donal Carroll, Chief Pharmacist, St. Luke’s Hospital, Kilkenny
• Ms. Sinead McCool, Senior Pharmacist & Project Lead, St. Luke’s Hospital, Kilkenny
• Ms Pauline Duggan, Pharmacist, Naas General Hospital
• Ms. Caroline Reidy, Hospital Key Account Manager, Pfizer Healthcare Ireland
• Mr. Jean Verschure, Director, Whathealth
• Mr. Chris Meehan, ICT Security Officer, Office of the CIO, HSE
• Mr. Richard Corbridge, CIO, HSE & Chief Executive of eHealth Ireland
• Ms Cliodhna Cotter, Pharmacist, Naas General Hospital
• Ms Fiona Ryan, Pharmacist, St. Lukes’s Hospital, Kilkenny
Project Team Picture:
(LtoR) Padraig Cahill, Pfizer Health Ireland; Richard Corbridge, CIO HSE & CEO eHealth Ireland; Sinead McCool, Senior Pharmacist and Project Lead, St. Luke’s hospital, Kilkenny; Caroline Reidy, Project Lead, Pfizer Healthcare Ireland; Marie-Claire Jago-Byrne, Chief Pharmacist and Project Lead, Naas General Hospital; Richie Stakelum, Portfolio Commercial lead, GIP, Pfizer Healthcare Ireland
*The software was licensed by Pfizer Healthcare Ireland to NGH and SLK for the purposes of this pilot in line with Pfizer’s internal donations’ policy and with the aim to advance knowledge in medicine, health care and allied sciences and science education and to improve the quality and availability of health care.
This study is an independent study undertaken solely by NGH and SLK, and neither Pfizer nor What Health has had or will have any input into the conduct or results of the case study. Furthermore, all statements and opinions in this document are those of the author and not those of WhatHealth or Pfizer.
Related file
- Ambulance Arrivals Project A Case Study
- SNOMED National Release Centre (NRC)
- SVUH Award winning Patient Flow Whiteboard
- Scan for Surgery
- Hospital-based care
- Digital Natives Sign App
- Digitisation of risk assesment tools for Adult mental health services in north Dublin
- Patient Engagement Operating Systems - Hep C
- Digital Transition for HSCPs at St. James's Hospital
- Primary Care Centre Castlebar Case Study
- Mario - Managing active and healthy ageing using caring service robots
- Claimsure - Health Insurance Claims Management System
- Cyber Attack Response
- Data systems in SVUH Emergency Department
- Electronic Discharge Prescription Pilot
- Epilepsy EPR
- eReferral
- eReferral Radiology Pilot
- eRostering
- Electronic Blood Tracking
- GP Practice Management Systems
- Healthmail
- Heart Failure Virtual Clinic
- Infrastructure - MPUP to ECAM
- IT Security - Small changes, big difference
- Kidney Disease Clinical Patient Management System
- Local Asset Mapping Project at St James' Hospital
- LUCY
- Mi Kidney App
- Model Community
- NCHD - Employment Record Portal
- Nursing & Midwifery Quality Care Metrics
- Ophthalmology Electronic Patient Record
- PharmaBuddy
- Radiology & Electronic Patient Record
- National Smart-Pump Drug Library of Paediatric and Neonatal Standardised Concentration Infusions
- Quality & Patient Safety
- Robotic Assisted Surgery Programme
- Shared Learning on EHR
- St. James' Hospital - National Haemophilia System
- Tallaght Hospital Pharmacy
- Tallaght Hospital Patient Engagement App
- Track & Trace
- Using IT to Improve Ireland's Public Sector Healthcare
- National Audiology Clinical Management System (NA-CMS)
- St Vincent's University Hospital Award Winning Whiteboard Patient Flow System
- Snomed Case Study
- Telehealth Project Donegal
- St Vincent's Whiteboard Patient Journey System a Case Study
- Ambulance Arrivals Project

